How two engineers are leveraging gene therapies to change the face of medicine
Human genes hold a wealth of information, including the ability to heal the body from within. Engineers throughout the College of Engineering continue to work to unlock the potential hidden within the science of gene therapy — the use of genetic information to treat diseases caused by genes, such as heart disease, cancer, diabetes and more. This experimental technique can be used to help manage or prevent diseases, and in some cases can even negate the need for drugs or surgery.
Protecting the World from Infection
According to the World Health Organization, lower respiratory infections — including influenza — are one of the top 10 deadliest diseases around the globe. Annually, influenza epidemics cause about 3 to 5 million cases of severe illness and between 250,000 and 500,000 deaths.
Philip Santangelo, professor in the Wallace H. Coulter Department of Biomedical Engineering, is principal investigator leading a team on research funded through a $21.9 million grant by the Defense Advanced Research Projects Agency (DARPA) seeking to develop better and faster responses to influenza strains.
Santangelo’s work uses gene modulation to turn on or off particular genes in the lungs, making them either more resilient against flu strains or stopping viral replication in its tracks.
“Flu vaccines are developed and administered every year, but they’re not always effective, and the disease has wide ramifications across the globe” says Santangelo. “Our research uses RNA-based techniques to manipulate what genes are expressed. For example, we can potentially turn off the receptor that allows the attachment of the flu virus to the epithelial cells inside the lung, stopping the infection process altogether.”
Santangelo hopes to eventually develop a drug that could be inhaled, using a version of human cells to protect against the flu. According to Santangelo, this drug should be widely applicable for a range of individuals, and potentially even different viral infections — including coronavirus.
“The first animal test takes place in early spring, and realistically this kind of therapy could be ready for a phase one human trial in the next four years or so,” said Santangelo.
“Flu vaccines are developed and administered every year, but they’re not always effective, and the disease has wide ramifications across the globe” says Santangelo. “Our research uses RNA-based techniques to manipulate what genes are expressed. For example, we can potentially turn off the receptor that allows the attachment of the flu virus to the epithelial cells inside the lung, stopping the infection process altogether.”
Optimizing Drug Delivery
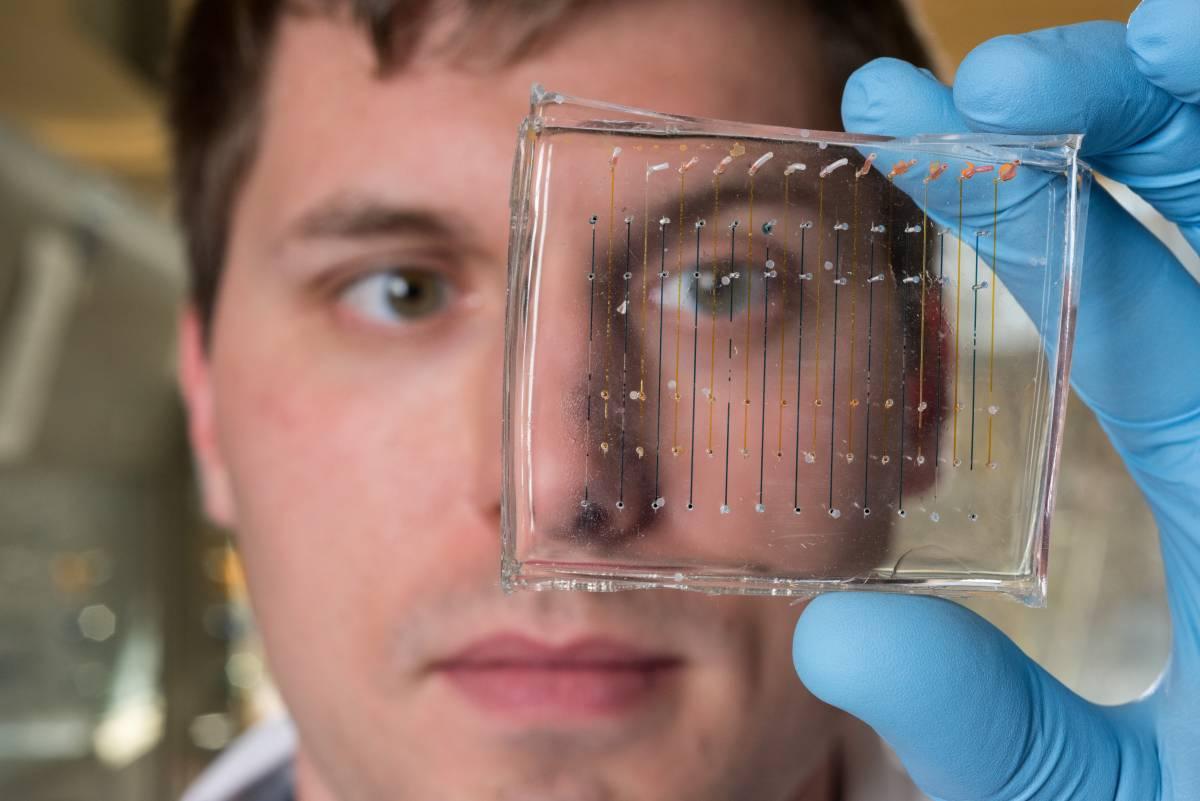
Because gene therapy is such a new technology, it can be challenging not only to develop an effective treatment, but also to administer it properly to patients. James Dahlman, assistant professor of biomedical engineering, is developing better delivery systems for gene therapy drugs made out of double-strand DNA or its molecular cousin, single-strand RNA.
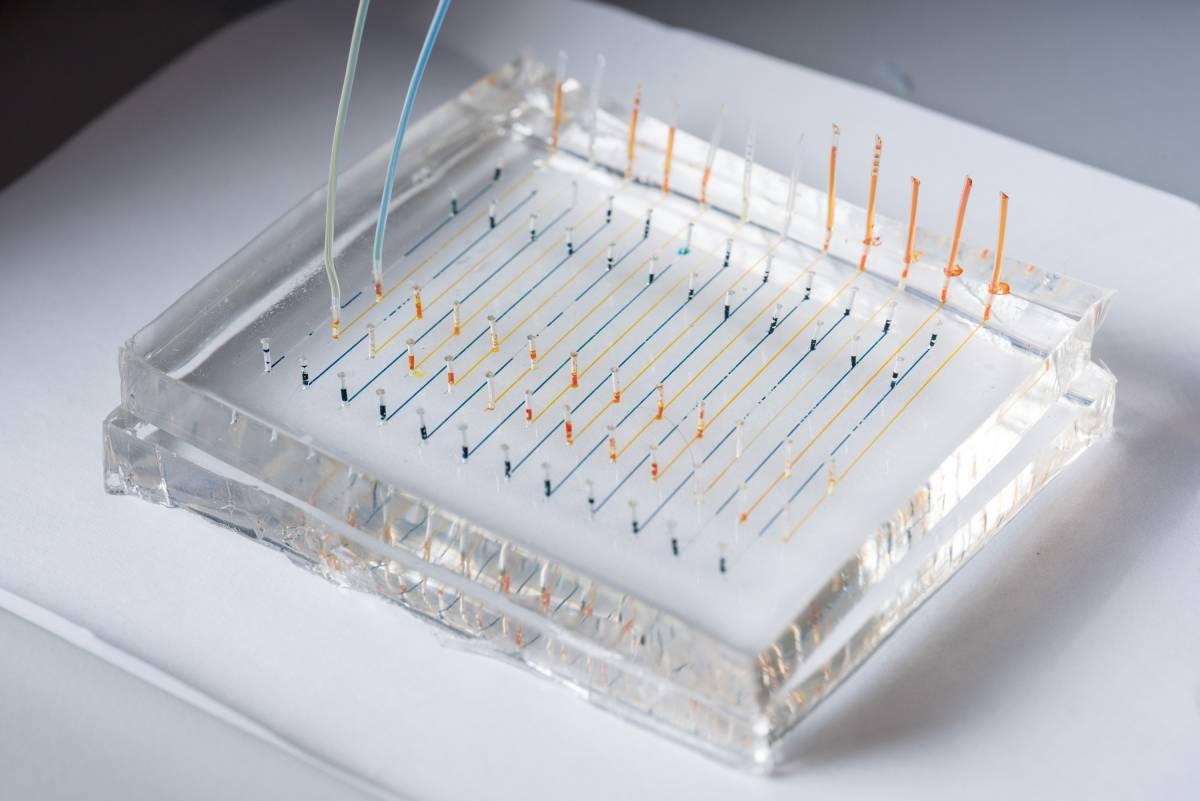
“Once these complex gene therapy drugs are created, it’s very difficult to get them directly to the diseased cells,” explains Dahlman. “My lab is creating nanostructured lipid carriers—basically tiny spheres about 50 nanometers wide made of fat molecules—that can be introduced to the body in order to deliver drugs to targeted cells, such as lungs, heart, or brain.”
For comparison, a human hair is approximately 90,000 nanometers wide.
These nanostructured lipid carriers can be injected — into the bloodstream, subcutaneously beneath the skin, or intramuscularly like a flu shot — or they can be nebulized into a mist and breathed in, similar to an asthma treatment.
Relatedly, one of Dahlman’s most impactful and renowned research projects is using similar nanoparticles in a variety of sizes and of different materials to find the best method by which scientists can deliver specific therapies to cells in the future.
This approach, known as DNA bar coding, was named one of the “Top 10 Emerging Technologies in the World” for 2019 by the World Economic Forum.
To test these nanoparticles for effectiveness, traditionally researchers would make thousands of different versions filled with the same drug and test them in vitro — that is, in cell culture dishes.
“The issue with this approach is that the delivery you get by spraying particles on cells sitting in a dish does not predict delivery that happens in living animals,” says Dahlman. “You are screening for nanoparticle candidates in a way that doesn’t predict what you want for an actual outcome.”
With Dahlman’s groundbreaking method, each different nanoparticle is labeled with a unique DNA barcode (instead of the drug being tested) and administered in vivo, or directly to the animal, isolating the appropriate cells, such as the spleen or lung.
Then, using gene sequencing, Dahlman and his lab can see exactly which nanoparticles did the best job of reaching the intended target. This approach allows researchers to choose the most effective particles of the bunch, infuse them with the gene therapy drug, and then administer them in animals to see the effects of the medication. By using DNA barcodes, the lab can perform hundreds of experiments simultaneously in a single animal. Gene sequencing allows researchers to move more quickly and efficiently towards implementing these therapies in the real world.
The Engineered Possibilities of Genes
The very first gene therapy approved by the U.S. Food & Drug Administration was a treatment for acute lymphoblastic leukemia in 2017; today, at least nine more have been approved for use in the U.S. on a variety of diseases, including a rare form of inherited blindness, spinal muscular atrophy, melanoma, and more.
Engineers like Dahlman, Santangelo and others in the Coulter Department of Biomedical Engineering are spearheading groundbreaking innovations and receiving recognition on a national scale. The study and manipulation of genes will continue to have an impact long into the future, especially the more researchers understand about these complex tools.